Introduction: When Images Lie
Radiology plays a critical role in diagnosing illness and injury. When a radiologist makes a serious mistake such as misreading an X ray or issuing a false negative report the results can be devastating. Radiology malpractice in Florida refers to these failures in diagnostic imaging that deviate from the standard of care and cause harm to patients.
This in depth article explains what constitutes radiology malpractice under Florida law, common radiological errors (like missed fractures, strokes, cancers, or internal bleeding on scans), the consequences for patients, and how Florida’s legal process addresses such cases. We also discuss real Florida malpractice cases involving radiology errors and how hospitals or clinics may be held liable.
What Is Radiology Malpractice Under Florida Law?
Radiology malpractice is a type of medical negligence. Under Florida law, medical malpractice occurs when a healthcare provider fails to meet the “prevailing professional standard of care” and injures a patient as a result. In simpler terms, malpractice means the radiologist did something (or failed to do something) that a reasonably careful radiologist would not have done under similar circumstances and that error caused harm.
Florida’s “Standard of Care” for Radiologists
The standard of care is a key concept in any malpractice case. Florida Statutes define it as “that level of care, skill, and treatment which, in light of all relevant surrounding circumstances, is recognized as acceptable and appropriate by reasonably prudent similar health care providers”. For a radiologist, this means interpreting imaging studies (such as X rays, CT scans, MRIs, mammograms, or ultrasounds) with the accuracy, diligence, and competence expected of a typical radiologist in that situation.
A radiologist’s duties include thoroughly reviewing images, identifying any abnormalities, and communicating critical findings promptly. Not every diagnostic miss amounts to negligence medicine isn’t perfect and some conditions are genuinely hard to detect. However, radiology malpractice occurs when the radiologist’s interpretation falls below expected standards.
Examples might include overlooking an obvious fracture on an X ray that most peers would catch, or misidentifying a telltale tumor on a CT scan that a prudent radiologist would recognize. In Florida, if such a breach of the standard of care leads to injury, it can give rise to a malpractice claim.
Common Diagnostic Imaging Errors (Misreads & False Negatives)
Radiologists are highly trained doctors, but they are not infallible. Diagnostic imaging errors occur more often than many realize in fact, diagnostic mistakes are one of the most frequent causes of malpractice claims. These errors can take many forms. Two of the most concerning types are misreads (incorrect interpretations of an image) and false negatives (failing to notice an abnormality, thus erroneously reporting the scan as “normal”). According to patient safety research, diagnostic errors including false negative readings on tests contribute to tens of thousands of deaths each year. Below we discuss some of the most common radiological misreads and false negatives, and how they happen:
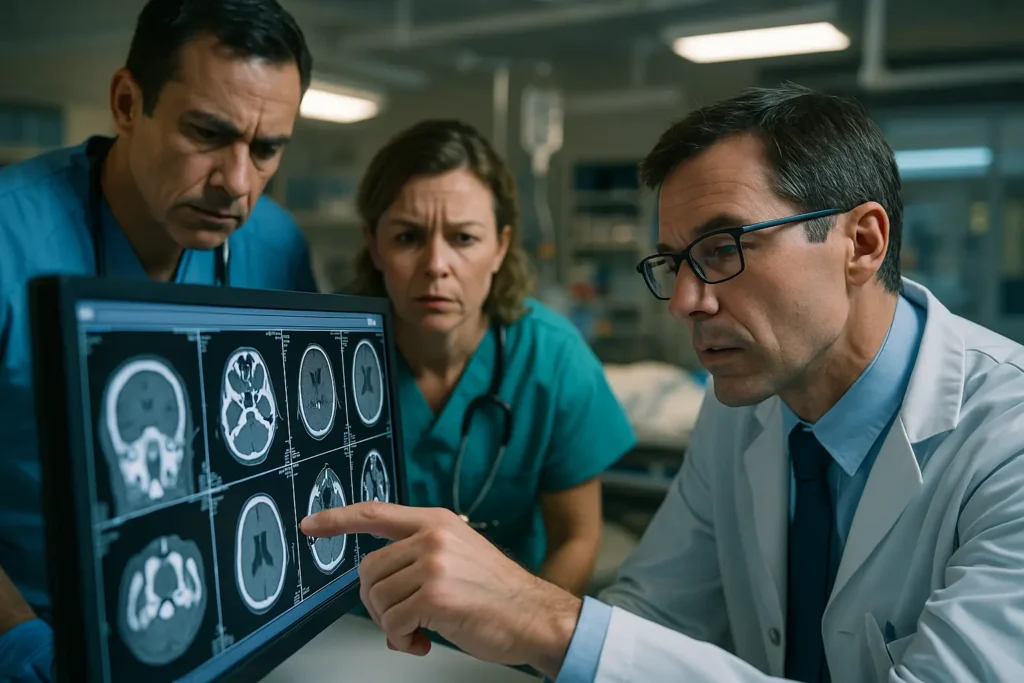
Missed Signs of Stroke on Brain Scans
Strokes are medical emergencies where minutes count. Radiologists play a critical role in stroke diagnosis by reading CT scans or MRI images of the brain to find bleeding (hemorrhagic stroke), clots or blocked arteries (ischemic stroke), or other signs of brain injury.
A stroke misdiagnosis can occur if the radiologist misreads the scan or delays reviewing it. Common errors include overlooking small areas of bleeding or subtle early signs of an infarct. In a fast paced ER setting, a radiologist might mistakenly conclude a brain scan is normal a false negative when in fact a stroke is evolving.
The consequences of missing a stroke on imaging are often tragic. Without prompt treatment (such as clot busting medication for an ischemic stroke or surgery for a bleed), the patient can suffer irreversible brain damage, paralysis, or death. For example, imagine a radiologist fails to detect a brain hemorrhage on a CT scan; if the patient is mistakenly treated as if they had no bleed (or even given blood thinners), it could cause catastrophic harm.
Likewise, if a radiologist doesn’t promptly communicate critical MRI results showing a blockage, a patient might miss the narrow window for effective clot busting treatment. Every minute of delay in stroke treatment can mean more lost brain function.
When a radiology error delays diagnosis of stroke, patients can be left with permanent disabilities such as speech loss, mobility impairment, or “locked in” syndrome, or their families may face wrongful death.
Misread X Rays and Missed Fractures
X rays are one of the most common imaging tests, used to detect fractures (broken bones), dislocations, or other injuries. A misread X ray occurs when the radiologist or attending physician fails to spot an abnormal finding on the film.
Some fractures like hairline cracks or small breaks in complex areas (e.g. spinal vertebrae or the neck) can be subtle. However, a reasonably careful radiologist should identify fractures that are evident. Missed fractures are a frequent subject of radiology malpractice claims.
If a broken bone is overlooked, the patient might be sent home without proper treatment (such as a cast, immobilization, or surgery). This can lead to improper healing, chronic pain, or even long term deformity or disability. For instance, if a cervical spine fracture (broken neck) is missed on a trauma patient’s CT scan or X ray, the patient could be at risk of spinal cord damage once the neck brace is removed.
There have been cases where patients became paralyzed after a missed neck fracture one jury awarded over $880,000 when a radiologist failed to spot a broken neck on a CT, leading to the patient’s quadriplegia.
Even less dramatic misses, like an undiagnosed wrist or ankle fracture, can result in arthritis, nerve damage, or need for later surgeries because the injury wasn’t stabilized early. Thus, misreading an X ray and sending someone away with an “all clear” when a bone is actually broken can cause significant harm.
Missed Cancer or Tumors on Imaging (False Negatives)
One of the most devastating radiology errors is failing to detect a cancerous tumor on an imaging study. Time is critical in cancer treatment a delay in diagnosis can allow cancer to progress from an early, treatable stage to a later stage that is much harder to cure. Radiologists are often the first line of defense in spotting cancers on tests like mammograms, chest X rays, CT scans, or MRIs. A false negative test in this context means the radiologist interprets the scan as normal or benign, and the cancer goes unnoticed.
Common Cancer Detection Failures
Missing a suspicious mass on a mammogram, overlooking a lung nodule on a chest X ray/CT, or misinterpreting a tumor as a “normal variant” on an MRI. Such errors can lead to delayed diagnosis of cancer sometimes by months or even years. Unfortunately, by the time the cancer is finally discovered, it may have grown or metastasized (spread) to other body parts.
Life Threatening Consequences
A patient who could have had a minor surgery or localized treatment might now face aggressive chemotherapy, major surgery like mastectomy, or have an incurable cancer because of the delay. For example, in one case a radiologist dismissed an abnormal thickening on a patient’s scan as benign; as a result, the patient’s Stage I cancer progressed to Stage IV and became terminal.
In Florida, a notable case in 2019 involved a radiologist who misread a woman’s breast imaging: he concluded a lump was not cancer when it actually was. About a year later, she was diagnosed with Stage IV breast cancer, which tragically was incurable by that point. A jury found the delay in diagnosis cut years off her life and awarded her $21.5 million in damages.
This shows how seriously such missed cancer diagnoses are viewed. Even when not fatal, a delayed cancer diagnosis can mean more extensive treatment (e.g. needing chemotherapy instead of just a lumpectomy) and a worse prognosis than if caught earlier.
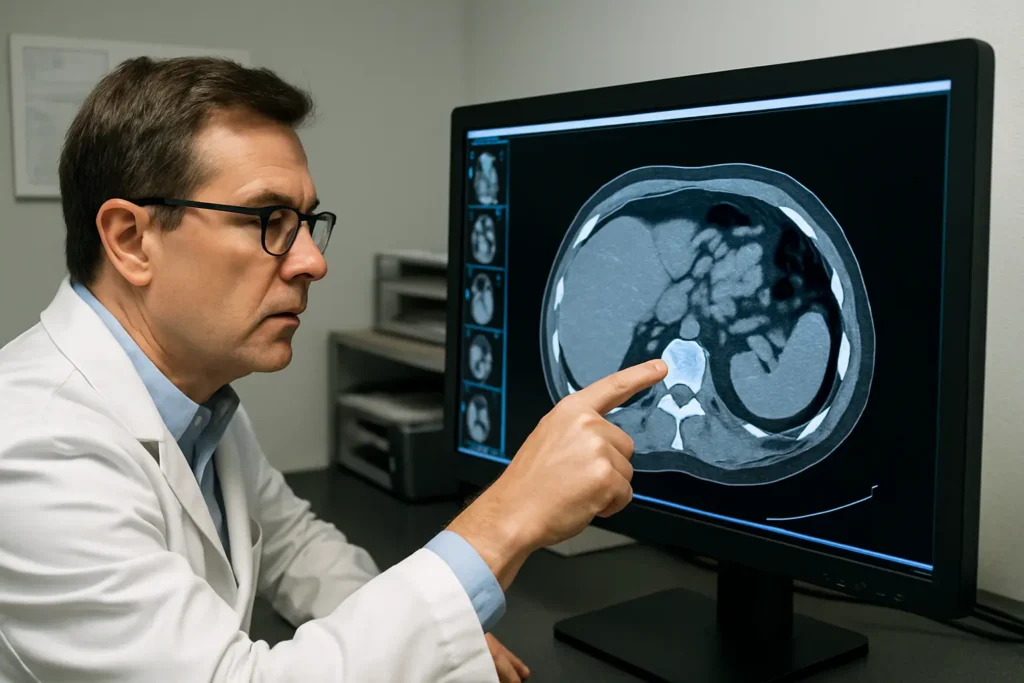
Overlooking Internal Injuries or Bleeding on Scans
Radiologists frequently assist in emergency settings by reading CT scans or ultrasounds for internal injuries for example, internal bleeding, organ damage, or other trauma. Missing a significant internal finding is another form of radiology error. For instance, after an accident or surgical procedure, a patient might have internal hemorrhage (bleeding) or an organ laceration. If a radiologist fails to identify blood pooling on a CT scan or misreads an ultrasound as normal, the patient may not receive urgently needed intervention.
Internal bleeding or organ injuries can rapidly become life threatening if not treated. A classic scenario is a radiologist overlooking signs of internal bleeding on an abdominal CT; if the bleed is left unchecked, the patient could go into hemorrhagic shock. In one documented case outside Florida, a feeding tube was misplaced into a patient’s lung; a radiologist then misread an X ray and failed to notice the tube had punctured the lung, resulting in the patient suffocating and dying hours later. While that case was in Georgia, it illustrates the kind of system failure that can occur: the radiologist admitted he breached the standard of care by missing the injury.
Even non fatal misses can cause great harm. Undiagnosed internal injuries may lead to infection, organ failure, or the need for more complex surgery later on. Radiologists also sometimes miss aneurysms (bulging blood vessels at risk of rupture) or intestinal perforations on scans conditions which, if not promptly addressed, can result in strokes or severe infections. Any imaging error that delays proper treatment of an internal injury puts the patient at risk of a much worse outcome.
How Radiology Errors Harm Patients: Delayed or Improper Treatment
When a radiologist’s negligence leads to a misdiagnosis or delayed diagnosis, the patient’s health can suffer in many ways. The potential consequences of radiology malpractice include:
Worsening of the Underlying Condition
If a condition like a fracture, hemorrhage, or tumor is missed, it continues to progress untreated. A small, hairline fracture might become a displaced fracture, or a small tumor might grow and spread. In stroke cases, a delay in recognizing a blockage or bleed means more brain tissue dies each minute leading to greater disability.
More Invasive Treatments Needed
Delays often mean that the patient, once finally diagnosed, faces harsher medical interventions. For example, a cancer that could have been removed easily when small might require chemotherapy, radiation, or extensive surgery after it grows. A missed internal injury that becomes infected might necessitate emergency surgery, whereas earlier it could have been managed less invasively.
Permanent Injury or Disability
Some radiology errors result in injuries that can’t be undone. Missing a spinal fracture or hemorrhage can lead to paralysis (as in cases where patients became paraplegic or quadriplegic due to missed findings). Missing a stroke may leave a patient with permanent brain damage, loss of function on one side of the body, or cognitive impairments that require lifelong care.
Wrong or Unnecessary Treatment
A radiology misread can also cause harm if it triggers the wrong treatment. A false negative (saying nothing is wrong) typically delays treatment, but a false positive (seeing a problem that isn’t there) can lead to unnecessary procedures. For instance, if a radiologist wrongly suspects a tumor that isn’t there, a patient might undergo an invasive biopsy or even surgery needlessly. Conversely, in stroke scenarios, misidentifying a hemorrhagic stroke as an ischemic stroke (or vice versa) can lead to giving contraindicated medications (like a blood thinner during a brain bleed) with disastrous results.
Emotional and Financial Toll
Beyond the physical injuries, patients and families experience emotional distress knowing that a medical oversight caused their suffering. There is also a financial impact: more treatment means more medical bills, time off work, rehabilitation costs, or in worst cases funeral expenses. Florida law allows malpractice victims to seek compensation for these economic and non economic damages (pain and suffering, loss of quality of life).
In short, a radiologist’s error can set off a cascade of negative outcomes. This is why diagnostic accuracy is paramount and why radiology malpractice cases often result in significant jury awards or settlements the harm caused is very real and often preventable. Medical studies have labeled diagnostic errors the “most common, catastrophic and costly” of malpractice incidents, estimating that they result in 40,000 to 80,000 hospital deaths in the U.S. each year. Florida patients who endure such errors have the right to seek accountability and compensation through a legal claim.
Examples of Radiology Malpractice Cases in Florida
Real world cases illustrate how radiology mistakes can cause life changing injury. Here are two notable Florida malpractice cases involving radiology errors:
Paraplegia from a Missed Spinal Injury $15.5 Million Verdict
One Florida case involved a patient, Jean Magloire, who became paraplegic (paralyzed from the waist down) after a series of radiology and diagnostic failures. Mr. Magloire had been in a serious truck accident and underwent leg amputation surgery. A few days later, he was still in the hospital when a radiologist performed a follow up CT scan of his spine. The radiologist, however, failed to notice critical findings on the scan specifically, a bone fragment in the spinal canal and an epidural hematoma (a pocket of bleeding near the spine) were present, but the radiologist did not flag them. He also did not recommend any further MRI to investigate. A neurosurgeon later reviewed the same CT but likewise failed to act on those abnormalities. As a result, the pressure on Mr. Magloire’s spinal cord went unrelieved and he became paraplegic (paralyzed).
When the case went to trial, the evidence showed that both the radiologist and the surgeon had breached the standard of care essentially, misreading the scan and not treating obvious red flags. The jury concluded that if the radiologist had properly identified the bone chip and hematoma, and the neurosurgeon had intervened, the paralysis could have been avoided. In the summer of 2019, a Florida jury awarded approximately $15.5 million in damages to Mr. Magloire and his wife for the immense harm caused by this misdiagnosis. This case underscores how a radiologist’s oversight in an imaging study can have dire, permanent consequences for the patient and how Florida juries will hold multiple providers accountable when their negligence combines to cause injury.
Terminal Cancer from a Misread Mammogram $21.5 Million Verdict
Another Florida case highlights the impact of a missed cancer diagnosis. In 2019, a Florida jury awarded $21.5 million to a woman whose breast cancer diagnosis was fatally delayed due to radiology errors. The plaintiff, a registered nurse, discovered a large lump in her breast and underwent imaging at the hospital where she worked. The radiologist performed an ultrasound and observed some skin thickening, but concluded the lump was benign, diagnosing it as likely mastitis (a breast infection) rather than cancer. He did not order a biopsy or properly image the lump itself, essentially giving a false negative. The patient was sent home on antibiotics.
About ten days later, still concerned, the woman sought a second ultrasound. Unfortunately, the technologist failed to capture clear images of the lump, and again the radiologist did not identify cancer. It wasn’t until roughly one year later after the lump persisted and grew that she was finally diagnosed with Stage IV breast cancer, which had metastasized. At that stage, the cancer was incurable, and doctors estimated she had only a short time to live.
The lawsuit alleged that the radiologist’s negligent misread of the imaging studies and failure to follow up on a clearly suspicious lump fell below the standard of care and deprived the patient of an early diagnosis that could have saved her life. Jurors agreed. They awarded $21.5 million, reflecting the lost chance of successful treatment and the suffering endured. This heartbreaking case demonstrates how diagnostic delays caused by radiologist negligence can literally be a matter of life and death. It also sends a strong message about accountability: even if cancer is a tough diagnosis, a gross oversight with such severe outcome will lead to a substantial verdict in Florida.
(These examples are drawn from publicly reported cases and illustrate the range of outcomes. Not every case will result in multi million dollar damages, but they show that Florida courts and juries take radiology errors very seriously when they cause significant harm.)
Pursuing a Radiology Malpractice Claim in Florida
If you or a loved one has been harmed by a radiologist’s mistake, you may wonder how to seek justice. Florida, like many states, has specific procedures for medical malpractice claims, including those against radiologists. It’s important to understand the legal steps and requirements, because Florida’s malpractice laws are complex and strict in procedural rules. Here’s an overview of how a radiology malpractice claim is pursued in Florida:
Pre Suit Investigation and Expert Affidavit
Florida law requires a presuit investigation before you can formally sue a healthcare provider for malpractice. This is outlined in Florida Statutes § 766.203. In practical terms, your attorney must consult a medical expert typically another radiologist in this kind of case who reviews the facts and determines that your claim has merit.
The expert will provide a verified written medical expert opinion, basically an affidavit stating that there are reasonable grounds to believe the radiologist was negligent and caused injury. This step acts as a certification that the case isn’t frivolous. Without an expert’s affidavit, a malpractice lawsuit cannot proceed in Florida.
Florida is quite specific about the qualifications of this expert. The expert generally must be a “similar health care provider” for a radiologist defendant, the expert should be a radiologist (or a physician with similar training in interpreting the same type of scans) who is actively practicing or teaching in the field. This ensures the opinion on the standard of care comes from a true peer. The expert’s written opinion is not filed in court right away, but it must be included when notifying the defendant(s) of the claim.
Notice of Intent and 90 Day Pre Suit Period
Before filing a lawsuit, the patient (through an attorney) must serve a Notice of Intent to Initiate Litigation on the allegedly negligent radiologist (and any other defendants, such as a hospital or clinic). This notice includes that expert affidavit and essentially informs the provider that you intend to sue for malpractice. Once the notice is sent, Florida law imposes a 90 day pre suit period (a waiting period) during which the claim is evaluated.
During these 90 days, the radiologist (or their insurance carrier and attorneys) must conduct their own investigation. The provider may forward your records to their own medical expert for review. By the end of the 90 days, the potential defendants have to respond in one of three ways: 1) reject the claim (deny liability), 2) offer to settle, or 3) offer to admit liability and go to arbitration on damages. If they reject the claim, they should provide their own expert affidavit stating why the care wasn’t negligent (essentially the mirror image of your affidavit, corroborating lack of negligence).
If no settlement is reached in that pre suit period (which is often the case), then you are legally allowed to file the malpractice lawsuit in court after the 90 days have elapsed. It’s critical to follow these steps to the letter failing to conduct the presuit investigation or serve proper notice can get your case dismissed. Florida’s pre suit process is designed as a hurdle to reduce frivolous claims and encourage early resolution of meritorious ones.
Filing the Lawsuit and Proving Your Case
After the pre suit requirements are fulfilled, your attorney files a formal complaint in the appropriate Florida circuit court. The complaint will outline the allegations, such as how the radiologist misread the imaging, how that was below the standard of care, and how it caused your injuries. From there, the case enters the normal litigation process: both sides engage in discovery (exchange of documents, depositions, expert reports, etc.), and eventually the case might go to trial if not settled.
To win a radiology malpractice lawsuit, the plaintiff must prove the same elements as in any negligence case: duty, breach, causation, and damages. In simpler terms:
Duty
The radiologist owed a duty to the patient (this is usually straightforward if the radiologist was interpreting your scan, a doctor patient relationship existed, establishing duty of care).
Breach
The radiologist breached the standard of care by acting (or failing to act) as a reasonably careful radiologist would. This is typically proven through expert testimony from another radiologist who explains how the defendant’s reading was incorrect or too hasty, etc., and why it constituted negligence.
Causation
That this breach caused harm meaning the error led to an injury that would not have happened otherwise. Causation can be a complex point, often requiring experts to link the delay or misdiagnosis to the worsened outcome. For example, an oncologist might testify that, more likely than not, the cancer would have been curable if caught earlier, but due to the delay it became terminal.
Damages
The patient suffered losses physical injury, additional medical treatments, pain and suffering, etc. as a result. Without damages, there is no case even if a mistake was made.
Florida has a two year statute of limitations for medical malpractice in most cases. This means you generally have two years from when you discovered (or reasonably should have discovered) the radiology error and injury to file the lawsuit. (There is also a four year overall deadline from the date of the malpractice, with a few exceptions, and a special rule for fraud or minors.) It’s important not to delay if you suspect an imaging misdiagnosis, because investigating and obtaining the necessary expert review takes time.
Given the technical nature of radiology malpractice cases, having qualified experts is absolutely vital. Often you will need a radiology expert to establish the breach, and other medical experts (neurologists, oncologists, surgeons, etc., depending on the injury) to prove causation and damages. A seasoned Florida malpractice attorney will know how to assemble this team and navigate the procedural hurdles, from pre suit through trial. The goal is to secure fair compensation for the injured patient covering medical expenses, lost wages, and the very real pain and suffering caused by the delayed or wrong diagnosis.
Hospital and Clinic Liability in Radiology Malpractice
When a radiologist is negligent, who else can be held responsible? In many cases, the radiologist isn’t the only party potentially liable. Hospitals, imaging centers, or clinics that employ radiologists (or contract with them) may also bear legal responsibility under certain theories. In Florida, two key concepts often come into play: vicarious liability (including apparent agency) and direct corporate negligence.
Vicarious Liability and “Apparent Agency”
Vicarious liability means an employer or principal is liable for the negligence of its employee or agent, if it occurred within the scope of their work. If a radiologist is an employee of a hospital or a radiology group, that entity can typically be sued as a co defendant. For example, if a hospital employed radiologist misreads a CT scan, the hospital itself may be vicariously liable for the malpractice. This is important because hospitals often have deeper insurance or assets to pay a claim than an individual doctor.
However, radiologists are frequently independent contractors rather than direct employees of the hospital. Historically, hospitals would try to avoid liability by saying the radiologist wasn’t their employee. Florida law has addressed this through the doctrine of “apparent agency.” In the landmark case Roessler v. Novak, a Florida court held that a hospital could be held liable for an independent contractor radiologist’s negligence if the radiologist appeared to be the hospital’s agent and the patient relied on that appearance. Essentially, if you go to Hospital X for a CT scan, and everything about the situation leads you to believe the radiologist is part of Hospital X’s team (which is a reasonable assumption for patients), the hospital cannot later dodge liability by claiming “oh, that doctor wasn’t our employee.” The hospital can be treated as if it employed the radiologist under an agency by estoppel or apparent agency theory.
In practical terms, most Florida hospitals now acknowledge they may be on the hook if the radiologist’s services were provided through the hospital to the patient. The focus is on the patient’s perspective: did the hospital “hold out” the radiologist as its agent (for example, providing radiology services in house without telling the patient the doctor is independent)? If so, the hospital and the radiologist may both be named in the lawsuit. This is particularly common in cases of emergency room malpractice involving radiology e.g., a patient in the ER gets an X ray read by an on call radiologist, misses a diagnosis, and the hospital ends up a defendant alongside the doctor.
Corporate Negligence and Administrative Failures
Apart from being vicariously liable for the radiologist’s actions, a hospital or clinic might have direct liability if the institution’s own policies or negligence contributed to the error. This is sometimes called corporate negligence or administrative negligence. Examples include:
Failing to Staff Adequately
If a hospital doesn’t have an appropriate radiologist available (e.g., no radiologist on duty overnight, or an overworked staff reading hundreds of films in a shift), mistakes can happen due to fatigue or delay. Not having qualified radiologists available in a timely manner can be seen as a breach of the hospital’s duty to its patients.
Poor Protocols or Communication Systems
Hospitals are supposed to have systems to ensure critical radiology findings are communicated promptly to the treating physicians. If a critical result falls through the cracks (for instance, the radiologist noted an abnormality in a report but no one followed up because the report was misfiled or not conveyed), the hospital’s communication failure could be deemed negligent. There are cases of “failure to communicate” in radiology leading to patient harm and hospital liability.
Negligent Credentialing or Supervision
A clinic or imaging center must hire competent radiologists. If a facility knowingly hires an unqualified practitioner, or continues to contract someone with a pattern of errors, it could be directly liable for negligent hiring/credentialing. Similarly, if a radiology practice fails to have double reading of certain high risk studies when it’s standard to do so, that could be a systemic issue.
In Florida stroke misdiagnosis cases, for example, not only might the radiologist be blamed, but plaintiffs often look at hospital protocol: Was there a timely read of the CT scan? Did the hospital have stroke alerts in place? Did they ensure results were communicated within minutes? If the hospital’s system was lax, the hospital itself can be at fault in addition to the individuals. One firm notes that liable parties beyond the radiologist might include the hospital that failed to maintain proper protocols or staffing to prevent such errors.
Likewise, administrative delays say, a radiology report not transmitted to the physician for several critical hours can make the facility liable if those delays stem from poor administration. Florida law recognizes that certain duties of hospitals (like emergency services) are non delegable, meaning the hospital must ensure they are carried out properly even if done by contractors. In essence, patient safety is a shared responsibility: the radiologist must do their job correctly, and the hospital/clinic must provide an environment that supports accurate and timely diagnoses. Failures on either end can lead to liability.
Empathy and Advocacy
If you are a patient who suffered due to a radiology mistake, it’s understandable to feel frustrated and anxious. You trusted the medical system to find and treat your problem, and instead you were let down. Florida’s malpractice laws exist to give injured patients a path to seek answers, accountability, and compensation. While no lawsuit can reverse a health tragedy, holding the responsible parties accountable can provide resources for your recovery and perhaps prevent future errors by driving improvements in care.
A compassionate and knowledgeable Florida malpractice attorney can evaluate your case including identifying all potential defendants (radiologist, hospital, etc.) and guide you through the legal process with your well being in mind.
Conclusion
Radiology malpractice in Florida is a serious issue that combines the complexities of medicine and law. Whether it’s a misread X ray leading to a missed fracture or a false negative CT scan delaying a critical diagnosis, the impacts on patients are often life altering. Under Florida law, radiologists are held to a high standard of care to diligently interpret imaging studies and when they fail, the law provides a remedy through malpractice claims. We have reviewed how common radiological errors happen, the devastating effects they can have (from worsened medical conditions to unnecessary surgeries or permanent disability), and the specific legal pathways Florida uses to address these wrongs.
If you or someone you love has been harmed by a radiology error, know that you are not alone. Similar cases have resulted in significant verdicts and settlements in Florida, indicating that juries understand the gravity of diagnostic mistakes. To pursue a claim, you must navigate Florida’s presuit requirements and prove the radiologist’s negligence with strong expert support. It can be a daunting process, but one aimed at securing justice and compensation for the injured patient.
Above all, our tone is one of clarity, authority, and empathy: you deserved accurate medical care, and when that didn’t happen, the law can help remedy the situation. While we hope you never face such circumstances, if you do, a qualified Florida medical malpractice law firm can offer guidance every step of the way. Your health and future matter, and holding negligent radiologists accountable not only helps you rebuild your life, but also encourages safer practices in the medical community moving forward.
Sources
- Florida Statutes § 766.102, defining “prevailing professional standard of care”
- Florida Statutes § 766.203, requiring presuit investigation and expert affidavit for medical negligence claims
- Freidin Brown, P.A. How to File a Malpractice Suit in Florida (explaining presuit, notice of intent, and 90 day period)
- Wilson v. Magloire case summary Florida radiologist’s misread CT leading to paralysis ($15.5 M verdict)
- Maryland Injury Law Center report of 2019 Florida $21.5 M verdict for missed cancer (radiologist’s false negative on breast lump)
- Bounds Law Group Orlando X Ray Misreadings (consequences of missed fractures, tumors, internal injuries)
- Bounds Law Group Radiologist Stroke Misdiagnosis (role of radiologist in stroke, examples of errors and liability)
- Boyers Law Group Radiologist Error Attorneys (common missed findings: aneurysms, ulcers, tumors, internal bleeding, etc., and resulting delays in treatment)
- Roessler v. Novak (Florida 2nd DCA) via Gordon Feinblatt LLC hospital liable for independent contractor radiologist under apparent agency
- Radiology Business news Georgia case of missed feeding tube injury (radiologist admitted misread; hospital still held liable)
- CRICO Strategies BMJ Quality & Safety study on diagnostic errors (21% of malpractice cases involve diagnostic error) and Society to Improve Diagnosis in Medicine data on deaths from diagnostic error
Attorney Bio: Jorge L. Flores, Florida Bar No. 53244, has been representing families in Miami Dade for over 30 years.
Disclaimer: This overview is general information, not legal advice. Deadlines and procedures can change based on facts and parties. For guidance on your specific situation, contact a Florida medical malpractice attorney.
