Introduction: When Laboratory Testing Fails
Pathology laboratories play a pivotal role in diagnosing diseases. Often, a single microscope slide or blood test can mean the difference between early life saving treatment and a missed illness. Pathology lab malpractice occurs when a lab or pathologist fails to meet the professional standard of care, leading to errors in diagnosis or testing that harm patients.
The consequences of these mistakes can be life altering or even fatal: a misread biopsy, incorrect cancer diagnosis, or lost lab sample can result in incorrect treatment, delayed care, or permanent injury. In Florida, where medical regulations are strict, such errors not only devastate families but also open the door to legal action aimed at accountability and compensation for the injured patients.
This page will explain what constitutes pathology lab malpractice, how these errors happen, real world examples (including Florida cases), and the legal process for pursuing a claim in Florida. The goal is to empower patients with knowledge. Understanding your rights can be the first step toward justice if you or a loved one has been affected by a lab’s negligence.
What Constitutes Pathology Laboratory Malpractice?
Pathology lab malpractice refers to serious mistakes in the collection, analysis, or interpretation of medical tests errors that fall below the accepted standard of care and directly cause patient harm. In practice, these errors often involve misdiagnosis or failure to diagnose a condition in a timely manner. Common examples include:
Misread Slides or Test Results
Perhaps the most classic pathology error is a misdiagnosis for instance, a pathologist examining a tissue biopsy under the microscope and concluding it’s benign when cancer is actually present (a false negative), or vice versa (false positive). In either case, the patient may undergo the wrong treatment: a missed cancer can progress without proper therapy, while a false cancer diagnosis can lead to unnecessary surgery or chemotherapy. Misinterpretation of cellular changes on slides is a core issue in many malpractice claims.
Delayed or Never Communicated Results
Even when lab findings are correct, communication breakdowns can amount to malpractice. If a lab discovers a critical result but fails to promptly report it to the treating physician or patient, life threatening delays in treatment can occur. For example, a Florida lab that doesn’t deliver a positive biopsy result in a timely manner may violate state requirements for timely reporting.
Such a failure to communicate can be catastrophic treatment is postponed or not initiated at all, allowing a condition to worsen needlessly. Under Florida law, healthcare providers (including labs) are required to share critical test results within specific timeframes; if they don’t, they can be held liable for resulting harm.
Specimen Handling Errors (Lost, Switched, or Contaminated Samples)
Laboratory malpractice often stems from breakdowns in basic procedures. A patient’s tissue sample or blood vial might be mislabeled with the wrong name or ID number, leading to another person’s results being assigned to them. Samples can even be mixed up or lost entirely. In other cases, poor handling can cause contamination for instance, a biopsy slide gets tainted by another specimen, yielding a false reading.
These errors are not mere clerical issues; they strike at the heart of diagnostic accuracy. A wrong label or mix up scenario can mean a sick patient is falsely told they’re healthy (because they received someone else’s clean results) or a healthy patient undergoes grueling treatments due to another person’s positive result. Such mistakes have been cited in Florida malpractice cases and are strong grounds for a claim, especially when proper labeling and chain of custody protocols were not followed.
Incorrect Test Processing or Analysis
Sometimes the testing process itself is flawed. Technical errors using the wrong type of stain on a slide, running an assay incorrectly, or mis calibrating a machine can produce incorrect results. A pathologist may also simply overlook an abnormality on a slide or report, perhaps due to fatigue or inadequate training. These kinds of lapses, where a competent professional would have identified the disease, constitute malpractice if they cause injury.
For example, missing unmistakable cancer cells on a slide that most pathologists would catch is a clear breach of the standard of care. In Florida, as elsewhere, the law doesn’t demand perfection from labs, but it does require reasonable competence if no careful professional would have made the same mistake, the pathologist or lab can be found negligent.
In essence, any deviation from the standard protocols or diagnostic accuracy that leads to patient harm might qualify as pathology lab malpractice. This could involve individual negligence (e.g. a pathologist’s misinterpretation) or systemic failures (e.g. a lab’s poor quality control or understaffing).
The key is that something the lab did wrong or failed to do directly caused a harmful outcome that would not have occurred with proper care.
How Do These Lab Errors Happen?
Understanding how these mistakes occur is important for both prevention and proving negligence. Errors in pathology and laboratory medicine typically arise from breakdowns at one (or multiple) stages of the diagnostic process. Experts often divide the lab testing process into three phases: the pre analytical phase, analytical phase, and post analytical phase. Each phase carries its own risks:
Pre Analytical Errors (Before Testing)
Studies show that the majority of lab mistakes some estimates say up to 70% happen before the sample even reaches a microscope or testing machine. This phase includes all the handling and preparation of specimens. It’s easy to see why errors here are so common. For example, mislabeling a specimen tube or slide with the wrong patient’s name is a simple human mistake that can have dire consequences, as discussed above.
Samples might also be stored improperly or transported under wrong conditions (e.g. not kept cold when they should be), causing degradation or contamination. In busy hospitals, there have been cases of samples getting lost or mixed up entirely. Rough handling can break or spill specimens. Any of these lapses can dramatically increase the risk of a diagnostic error.
Even small mix ups matter as one report cited by the Florida Department of Health noted, about 1% to 5% of results in clinical labs might contain some inaccuracy. That sounds low, but across thousands of tests, it means many patients could be affected each year by preventable mistakes.
This is why Florida imposes strict regulations on laboratories (such as Florida Administrative Code Rules 59A-7 and 64B-3) regarding sample handling, labeling, and quality control. When labs cut corners on these protocols, the likelihood of malpractice rises.
Analytical Errors (During Testing and Interpretation)
The analytical phase is when the test or analysis is actually performed for example, when a tissue slide is examined under the microscope or a blood sample is run through a machine. Errors here can stem from equipment malfunction or calibration problems (a machine that isn’t properly calibrated could output incorrect values), technical mistakes by the lab technician (like using the wrong reagent or procedure), or the pathologist’s own misreading of a slide or data. While modern laboratories use advanced technology and standardized procedures, they are not foolproof human oversight is crucial, and human error can still occur.
For instance, a pathologist might miss a small tumor in an imaging scan or mistake an abnormal cell for a benign artifact. These professional interpretation errors are at the core of many pathology malpractice cases (e.g., a cancer on a biopsy that one pathologist fails to see but any reasonably careful specialist would have spotted). Such mistakes often come to light only later, when a patient’s condition worsens and a second review reveals the earlier oversight.
It’s worth noting that pathology is sometimes as much art as science certain cases are genuinely difficult or ambiguous. But malpractice law targets the clear cut failures: those situations where an average qualified pathologist would have made the correct call under the circumstances.
Post Analytical Errors (Reporting and Follow Up)
Even after a test result is obtained, there’s potential for error in how results are reported and acted upon. A classic post analytical error is delayed or failed communication the lab generates a report but it doesn’t reach the doctor or gets buried in paperwork. Florida has specific rules requiring labs and healthcare providers to timely communicate “critical” findings to the treating physician (for example, a malignant biopsy finding). If a lab report sits for weeks without being sent out, that’s a serious breach.
Other post analytical issues include clerical errors in reports (like a positive result accidentally typed as “negative”), or a clinician misinterpreting an overly technical lab report without seeking clarification. However, these latter issues often overlap with physician error rather than lab malpractice. From the lab’s perspective, the most direct post analytic duty is to ensure accurate, clear results are delivered promptly to the right recipients.
When that doesn’t happen, patients can suffer “errors of omission” no one acts on a life threatening lab finding because it fell through the cracks. For example, if a pathology report confirming cancer is sent to the wrong fax number and the patient is never told, the delay in treatment could be devastating.
Such scenarios absolutely underpin malpractice claims. As one Florida law firm noted, failure to communicate results is a frequent basis for lab negligence lawsuits, because a critical delay can make the difference between a treatable condition and a terminal one.
By examining how an error happened, investigators can identify who is liable. Was it a negligent technician who mixed up samples? A pathologist who rushed and missed obvious disease markers? Or a systemic failure, such as inadequate processes or understaffing at the lab? In many cases, it’s a combination.
Florida labs are required to have quality assurance measures, but when those measures fail or are ignored patients pay the price. Understanding the origin of the mistake is also critical legally, because it helps establish the “breach of duty” (what specifically was done wrong) in a malpractice case.
Real World Examples of Pathology Malpractice
Real case stories help illustrate just how serious pathology errors can be. Unfortunately, Florida has seen several high profile incidents of lab malpractice with dire outcomes:
Misread Pap Smear Leads to Late Stage Cancer
One notable case involved Darian Wisekal, a 37 year old Florida woman and mother of two. She underwent routine Pap smear tests (which screen for cervical cancer) in 2008 and again in 2011, and both slides were erroneously read as negative by the LabCorp laboratory.
In reality, she had cervical cancer that went undiagnosed during that period. By the time it was finally discovered, the cancer was advanced. Darian tragically died of cervical cancer in 2011 three years after that first “all clear” result. Her husband sued LabCorp for negligence, arguing that any competent cytologist would have detected the cancer cells.
In 2014, a federal jury agreed and found LabCorp 75% at fault for her death, awarding the family approximately $15.8 million in damages. (Some blame was assigned to Mrs. Wisekal’s doctors as well, hence LabCorp’s 75% share of fault.)
The case highlighted how a misread slide can literally cost a patient her life. Internal records showed the 2008 Pap slide had abnormalities that were overlooked. The jury’s verdict sent a strong message: labs must take the time to do it properly, because people’s lives “are passing by” on each slide.
Although an appeal later reduced the noneconomic damage award, the liability finding underscored the grave consequences of a false negative error. This case also showed how Florida’s comparative negligence works even if others (or the patient) are argued to share in the fault, the lab can still be held largely accountable when its error is a substantial factor in the harm.
Cancer “Missed” on a Biopsy A Life Cut Short
Another example is the case of Rex Morgan, a Jacksonville, Florida basketball legend (a former Boston Celtics player and local high school coach). Mr. Morgan had survived a bout of throat (tonsil) cancer in 2010. During his follow ups, a biopsy of a new tongue lesion in November 2011 was sent to Quest Diagnostics for analysis.
The Quest pathologist’s report came back “no malignancy identified”, suggesting the lump was benign (possibly a fungal infection). Relying on that, doctors did not treat for cancer at that time. Sadly, about two years later, in 2013, Rex’s cancer roared back a subsequent biopsy in early 2014 revealed invasive cancer in the same area of the tongue. Despite aggressive treatment, he died in January 2016.
After his death, independent experts re examined the original 2011 biopsy slides and found cancerous cells that the first pathologist had missed. In 2016, Mr. Morgan’s widow filed a wrongful death lawsuit alleging Quest’s pathologist negligently misread the slide and that, had the cancer been caught in 2011, her husband’s life could have been saved with timely treatment.
This kind of error a false negative biopsy meant a critical head start against cancer was lost. The case is a somber reminder that even renowned labs like Quest are not infallible. A local pathologist not involved in the case told news media that around 1% of biopsies are misdiagnosed in general, acknowledging that differences in opinion can occur in tricky cases.
However, the Morgan case appeared to be more than a reasonable difference experts said the tumor was “well differentiated” (slow growing) and should have been spotted earlier. For Mrs. Morgan, the outcome was devastating: “By missing that, they cost him his life,” she said of the lab’s error.
This case underscores that when a lab’s mistake leads to delayed diagnosis, the law will question whether the oversight was one a careful professional should have avoided. If not, it’s malpractice.
False Cancer Diagnosis with No Actual Harm
Not every lab error results in physical injury but even those “near miss” scenarios highlight Florida’s legal strictness. Consider a recent Florida incident where a woman was wrongly told she had cancer based on a botched lab test, when in fact she was cancer free.
She and her husband endured two months of profound emotional anguish, believing she was terminally ill; they canceled a dream vacation, started “preparing” for the end, and she underwent unnecessary medical expenses and stress. Ultimately, a second opinion at a specialty center showed the lab’s diagnosis was mistaken essentially a false positive.
One might assume such a grievous error would be grounds for a lawsuit. However, Florida law is very strict on requiring actual injury. Because, in this case, the woman fortunately did not undergo harmful treatment or suffer a physical injury before the mistake was corrected, she found that she had no viable malpractice claim for the emotional distress and life disruption caused by the false diagnosis.
As one Florida attorney explained, the state rarely provides legal recourse for patients who experience a misdiagnosis if it’s corrected in time to avoid permanent injury or death. The cost of pursuing a malpractice suit (which requires expensive expert witnesses and lengthy litigation) is so high that without a significant tangible injury, no lawyer could take the case any damages would be mainly for emotional harm, which juries are hesitant to award in large sums when the patient ended up “okay” health wise.
Instead, the woman filed a complaint with regulatory authorities, but she could not obtain compensation for the nightmare she was put through.
This example, though not a traditional success story, is instructive: it shows that Florida’s malpractice system centers on cases with clear physical harm or significant damages. Emotional trauma alone, while very real, may not meet Florida’s threshold for a viable claim. In a sense, it’s a perverse silver lining if a lab error nearly caused tragedy but disaster was averted, the law may leave the patient to bear their own costs (a fact many find frustrating).
These scenarios demonstrate the stakes of pathology errors. Whether it’s a false negative delaying a critical treatment or a false positive subjecting someone to fear and unnecessary interventions, the human impact is enormous. Cancers advance unchecked; patients undergo wrong surgeries or endure needless pain; families lose loved ones or suffer anxiety that can never be fully undone. That’s why the legal system allows those harmed to seek accountability.
When a pathology lab fails in its duty and a patient is harmed or lost, a malpractice lawsuit can not only provide compensation but also drive changes in lab practices. Many labs have improved procedures (such as requiring a second pathologist’s review for certain test results) as a direct response to errors and subsequent legal cases.
The overarching lesson from real cases is clear: accuracy in the lab saves lives, and when labs fall short, Florida law provides a path to seek justice albeit with stringent requirements.
Pursuing a Pathology Malpractice Claim in Florida
Florida’s legal framework for medical malpractice is one of the more complex and demanding in the nation. The state has instituted strict pre suit procedures, specific qualification rules for experts, and tight deadlines for filing claims.
This means that if you suspect you’re a victim of lab malpractice in Florida, it’s crucial to understand the road ahead. In this section, we break down the key steps and requirements for pursuing a pathology lab malpractice case in Florida, and what you as an injured patient or family member need to prove for a successful claim.
Proving Negligence: Four Elements of Malpractice and the Burden of Proof
Like all medical malpractice cases, a pathology error claim is fundamentally a negligence case. This means your legal team must prove four essential elements to prevail:
Duty of Care
You must show that the defendant owed you a duty. In a lab context, this is usually straightforward the pathologist or laboratory had a professional obligation to properly handle and interpret your specimen. When a hospital or doctor sends your biopsy or blood test to a lab, that lab takes on a duty to you to perform the analysis with the level of care and skill that a reasonable lab in the same situation would use. In Florida, laboratories and their personnel (e.g. pathologists, lab technologists) are considered healthcare providers, so they owe patients this duty under medical standards.
Breach of Duty
Next, you must prove that the lab or pathologist breached that duty by failing to meet the applicable standard of care. The standard of care is essentially what a competent professional would have done (or not done) in the same circumstances.
For example, given a certain microscope slide with evident cancer cells, the standard of care for a pathologist would be to recognize and report the cancer. If a pathologist misses it and especially if most peers would not have that’s a breach.
Likewise, losing a specimen or mixing up patient samples is a breach because a reasonably careful lab with proper procedures would not make such a mix up.
This element often hinges on expert testimony: an expert pathologist can explain how the defendant’s actions deviated from accepted practices.
Florida law requires that the provider’s actions be compared against those of “similarily qualified” professionals e.g., a board certified anatomic pathologist’s work is measured against what a typical competent board certified pathologist would do. Any action or omission that falls below that benchmark is negligence.
Causation
Proving breach isn’t enough; that breach must have caused an injury. Causation in malpractice means showing that, more likely than not, the harm you suffered was a direct result of the lab’s error. In other words, had the mistake not occurred, you wouldn’t be injured (or your prognosis would be better).
This is sometimes contested fiercely. For instance, a lab might admit it misread a slide, but argue that even a correct diagnosis at the time wouldn’t have changed the outcome (perhaps the cancer was already incurable, or the patient’s own actions contributed). In the Wisekal case, LabCorp tried to argue that even if they’d identified abnormalities, the cancer might not have been diagnosable or treatable at that stage. The jury rejected that, finding the delay did worsen her outcome.
To prove causation, your lawyer will often rely on medical experts who can say, for example, “If the cancer had been diagnosed in 2011, it likely could have been successfully treated because it wasn’t, the patient’s chance of survival dropped dramatically, leading to her death.” It establishes that the lab’s mistake was a substantial factor in the harm. Under Florida’s standards, causation must be shown to a reasonable degree of medical probability.
Damages
Finally, you must have suffered damages some quantifiable loss as a result. In a pathology error case, damages can be severe: the cost of additional or more intense treatment due to a delay, the physical pain and disability from a worsened condition, lost income, or the tragic loss of life (which leads to a wrongful death claim for the family). There are also non economic damages like mental anguish, pain and suffering, loss of capacity to enjoy life, etc.
Florida law requires that a plaintiff show actual injury; as noted in the misdiagnosis example above, if the error was caught early enough that no lasting harm was done, there is effectively no case because the damages element fails. But when real harm does occur, Florida allows recovery of a wide range of damages (with some statutory limitations discussed later).
The injured party needs to document these losses medical records, bills, expert evaluations of future medical needs, testimony about pain and suffering, and so on.
All four elements duty, breach, causation, and damages must be proven by the “greater weight of the evidence” (more likely than not) in order to win a malpractice lawsuit. The burden of proof lies with the patient (plaintiff).
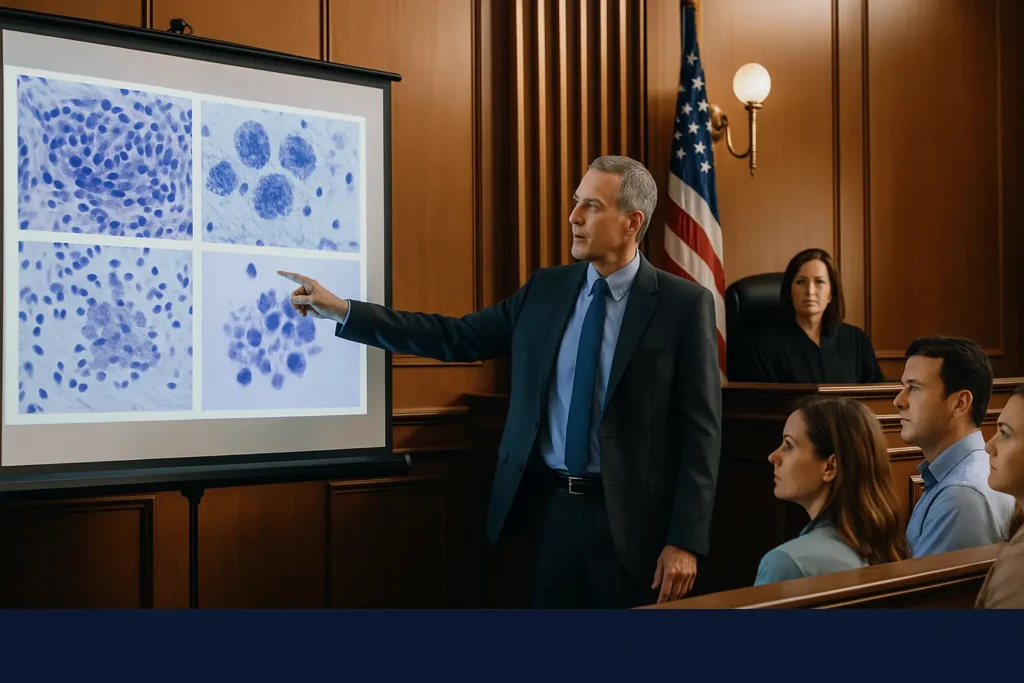
Given the technical nature of pathology, this invariably requires expert testimony. In fact, Florida law makes expert support mandatory in med mal cases: “In Florida, expert testimony is not just helpful it is legally required in medical malpractice cases.” Without a qualified medical expert affirming that malpractice occurred, the case can be dismissed at an early stage.
Typically, you will need at least one expert pathologist (or related specialist) to testify that the lab’s conduct fell below standard and caused the injury. This expert essentially educates the jury on what should have happened versus what went wrong. They might say, “No reasonable lab technician would mistake these cells for benign,” or “The lab failed to follow standard labeling protocol, which any careful facility would have done, and that led directly to the patient getting the wrong results.”
Florida sets specific qualifications for these experts generally, the expert must practice (or have practiced) in the same specialty and have familiarity with the type of case (for example, a board certified pathologist to critique another pathologist’s work). The reliance on experts can’t be overstated: they are the linchpin of proving breach and causation. Florida juries are instructed to weigh expert opinions, and a persuasive, credentialed expert can make the difference in meeting your burden of proof.
Florida’s Pre Suit Requirements: Expert Affidavit and Notice of Intent
Florida has a unique pre litigation process for medical malpractice claims that is designed to weed out frivolous cases and encourage early resolution. Before you can even file a malpractice lawsuit in court, you must navigate these steps. The process can be summarised as follows:
Pre Suit Investigation & Expert Affidavit
Florida Statutes § 766.203 and § 766.204 require that a prospective malpractice claimant conduct a reasonable investigation into the merits of the claim and obtain a written medical expert opinion corroborating that there are grounds to sue.
In practice, this means your attorney must consult with a qualified medical expert (usually in the same field as the alleged negligence) who reviews the records and signs an affidavit or written statement swearing that, in their expert opinion, the lab or pathologist’s care fell below the standard and caused injury.
This is often called an “affidavit of merit” or a “verified medical expert opinion.” It’s essentially a gatekeeping requirement Florida wants a medical professional to vouch that your case has legitimacy. Without this affidavit, you cannot proceed. Your lawyer will typically gather medical records (pathology reports, slides, treatment records) and present them to an expert for review.
Only if the expert concludes malpractice likely occurred will they sign off on the affidavit. This step is crucial and can take time, because finding and consulting with the right expert is involved. However, it’s non negotiable: Florida law mandates an expert affidavit at the outset of a malpractice claim.
Notice of Intent to Sue
Once the expert opinion is in hand, the next step is to provide notice to the potential defendants. Florida Statute § 766.106 requires that you serve all prospective defendants (the lab, the pathologist, and any other health provider you intend to sue) with a Notice of Intent to Initiate Litigation at least 90 days before actually filing the lawsuit.
This notice must be sent by certified mail and should include a brief description of the claim, the alleged negligence, and the injuries, along with the supporting expert affidavit and an authorization for the defendants to obtain relevant health records. Essentially, you are telling the lab “We intend to sue you for malpractice, here’s why, and here is an expert who agrees that you were negligent.”
When the notice is served, it triggers a 90 day pre suit period during which the lawsuit itself is on hold. This is a mandatory waiting period designed for investigation and potential settlement discussions. The statute even tolls (pauses) the statute of limitations during these 90 days. During this time, the lab’s insurance company and lawyers will investigate the claim.
They might request informal discovery Florida’s pre suit rules allow for document exchanges, written questions, and even unsworn statements from the parties during this period.
As a claimant, you and your attorney must cooperate with reasonable information requests (and the defense must reciprocate) so that everyone can evaluate the claim’s merits. By the end of 90 days, the prospective defendant must respond in one of three ways: (1) reject the claim (deny liability), (2) offer to settle, or (3) offer to admit liability and go to arbitration on damages. If they deny or the period expires with no resolution, you are then free to file the formal lawsuit in court.
This whole pre suit phase is essentially a dance to see if the case can be resolved or should proceed to litigation, and to ensure that claims have expert support. It’s a bit of a minefield procedurally a mistake in the notice (like failing to include the right medical records or proper authorization forms) can derail a case. Therefore, having a knowledgeable Florida malpractice attorney handle this is extremely important.
From a patient’s perspective, the pre suit process can be frustrating it adds a delay (at least 90 days, often longer with extensions) before you can get your day in court. But it’s the law’s way of forcing both sides to evaluate the case early. Some cases do settle in this phase if the lab’s liability is clear.
Others are denied, which then allows the plaintiff to file suit and formally begin litigation. Keep in mind, the expert affidavit that you obtained is not automatically shared with the jury or anything, but it’s effectively your ticket to file the lawsuit. If you fail to secure the affidavit or properly complete the pre suit steps, a judge will dismiss your case for not complying with conditions precedent under Florida law.
Statute of Limitations and Deadlines
Florida has strict deadlines for filing malpractice claims. Generally, a medical malpractice (which includes lab errors) lawsuit must be filed within 2 years from the time the patient (or family) discovered the injury or reasonably should have discovered it, but no later than 4 years from the date of the malpractice incident. This dual deadline is known as the statute of limitations (the 2 year rule) and the statute of repose (the 4 year outer limit).
For example, if a pathology error occurred on January 1, 2020, and the patient discovered it on January 1, 2021, the 2 year clock would start at discovery (2021) and thus expire on January 1, 2023 which is within the 4 year absolute cutoff of January 1, 2024. However, if the error wasn’t discovered until year 3 or 4, the patient might bump into the 4 year repose limit, which can bar the claim even if they had no idea of the malpractice until later.
Florida does have a limited fraud exception: if the provider engaged in fraud or intentional concealment that prevented discovery of the malpractice, the period can extend up to 7 years from the incident. There’s also an exception for minors: if the patient is a child, the statute of limitations may be tolled until they reach the age of majority (with some conditions). In the context of pathology, delayed discovery is common you might not find out an error occurred until months or years later when a correct diagnosis finally comes in.
Florida’s 2 year from discovery rule is therefore critical. As soon as you suspect a lab mistake caused you harm, the safest course is to assume the clock has started ticking. The 90 day pre suit notice period tolls (pauses) the limitation period once you send the notice, and you can also petition for an automatic 90 day extension to investigate a potential claim if you need it. But these are technical maneuvers best handled by an attorney.
The bottom line: timing is critical. If you miss the deadline, you’ll likely be barred from suing at all, no matter how strong your case. As one Florida legal guide bluntly puts it, a victim of malpractice must act promptly or risk losing their rights. If you’re even contemplating that a pathology error harmed you, consult counsel early to protect your ability to file.
The Role of Expert Witnesses in Pathology Cases
Expert witnesses deserve special mention, because in pathology malpractice cases they are truly the linchpin of success. Pathology is a highly technical field, and jurors (and judges) are usually laypeople with no medical training.
An expert witness typically a board certified pathologist or another laboratory medicine expert will be called upon by the plaintiff to explain exactly how the error occurred and why it was a deviation from the standard of care. They essentially “translate” the medical details into understandable terms and offer their professional opinion that the defendant messed up.
In Florida, as noted, you cannot even file suit without an initial expert affidavit. But that same (or another) expert will usually later provide deposition and trial testimony as the case progresses. Their tasks include:
Identifying Diagnostic Failures
An expert will review the same slides, lab reports, and data that the original pathologist did. They might point out, for example, cancer cells on a slide that were clearly visible and should have been recognized. Or they might examine lab procedures and say, “Given the protocols, this sample mix up would not happen unless someone breached protocol.” Essentially, they establish what went wrong from a professional standpoint.
Establishing the Standard of Care
The expert educates the court on what a reasonably prudent lab or pathologist should have done. For instance: “Any biopsy showing XYZ pattern should be subjected to a second review” or “The standard is to double check patient identifiers on specimens; failing to do so is a breach.” By doing this, they create a baseline against which the defendant’s actions are measured.
Linking the Error to Harm (Causation)
An expert also gives opinion on causation. For example, a pathology expert or perhaps a treating oncologist might testify that a one year delay in diagnosis allowed a cancer to progress from Stage I to Stage III, significantly worsening the patient’s prognosis thereby directly tying the lab error to the injury (advanced disease). Or an expert could explain that a patient underwent a painful, disfiguring surgery only because of a false positive lab result, meaning the lab error caused unnecessary harm. This testimony helps the jury connect the dots from negligence to damage.
Florida’s laws also impose requirements on who can serve as a medical expert in malpractice cases. Generally, the expert must practice (or have recent practice) in the same specialty and be familiar with the standards of care for that specialty.
In pathology cases, this means your expert should ideally be a pathologist with experience in the specific branch of pathology at issue (e.g., cytology for a Pap smear case, surgical pathology for a biopsy case). The defense, of course, will likely have their own expert who may claim that the error was an understandable mistake or that it didn’t breach the standard of care. Thus, often a battle of experts ensues. But without a supporting expert, the plaintiff’s case cannot get to a jury.
It’s worth noting that Florida not only requires experts, but is also particular about them. For example, if the defendant is a board certified specialist, your expert must usually be board certified in the same specialty.
There are also statutes about out of state experts and pre trial vetting of experts. This is why in high stakes cases, law firms often engage top tier pathologists from around the country to consult. As mentioned earlier, some Florida firms maintain networks of leading experts ready to review complex pathology issues. That level of expertise can be crucial, especially if the case involves nuanced or rare diseases.
In short, expert witnesses are the backbone of a pathology malpractice case. They provide the scientific authority that allows a jury to confidently determine that negligence occurred. For the injured patient, having a credible expert effectively “on your side” is empowering it validates that what you experienced wasn’t just bad luck but substandard care. Florida’s system acknowledges this by mandating expert involvement from start to finish.
Compensation for Victims of Lab Malpractice
A successful pathology malpractice claim in Florida can result in financial compensation for a variety of losses. While no amount of money fixes the health consequences of a misdiagnosis or delay, compensation serves two purposes: it helps cover the economic burden and it acknowledges the intangible suffering endured.
If you prevail (or settle) in a lab malpractice case, you may be entitled to recover:
Economic Damages
These are the tangible financial losses. They include medical expenses for treating the worsened condition (for example, the cost of extra surgeries, chemotherapy, or extended hospital stays that would have been avoided with a timely diagnosis).
Future medical expenses related to the harm are also covered if a delay caused a permanent disability requiring ongoing care, the projected cost of that care can be claimed. Lost income is another major economic damage: if you had to stop working or lost wages due to your illness or its treatment, those losses can be reimbursed.
In the case of a wrongful death, economic damages might include the family’s loss of the decedent’s financial support. Florida law allows plaintiffs to claim lost earning capacity as well if a preventable error reduced your ability to work in the future, the value of that lost earning potential is compensable. These damages are often substantiated by medical bills, actuarial calculations, and expert economic testimony.
Non Economic Damages
These refer to more subjective, human losses pain, suffering, mental anguish, loss of enjoyment of life, and so on. Suffering a needless progression of cancer, for example, brings immense physical pain and emotional distress. Florida Statute § 766.118 defines non economic damages in malpractice cases and (as of the last update) places certain caps on them in practitioner negligence cases.
Historically, Florida had a $500,000 cap per claimant for non economic damages in medical malpractice personal injury cases (and $1 million in some wrongful death or catastrophic cases), though these caps have been the subject of legal challenge and are not applied in the same way after court rulings.
(In 2017, the Florida Supreme Court struck down caps in personal injury malpractice cases, finding them unconstitutional, though caps in wrongful death cases had already been invalidated in 2014.)
Therefore, the landscape on caps is complex but generally, plaintiffs can still seek significant non economic damages, and egregious cases sometimes result in very high jury awards for these losses (as seen in the initial $15 million noneconomic portion of the Wisekal verdict, which was later judicially reduced). It’s important to have a skilled lawyer who knows the current law on damages.
Wrongful Death Damages
If the malpractice resulted in a patient’s death, Florida’s Wrongful Death Act comes into play. The surviving family (spouse, children, and in some cases parents) can recover damages for their own losses, such as loss of companionship, mental pain and suffering from the date of injury, and the value of support and services the deceased provided. They can also recover the deceased’s medical expenses and funeral costs. One heartbreaking aspect of cases like Wisekal’s or Morgan’s is that families are left not only grieving but also often financially destabilized; wrongful death damages aim to alleviate that financial impact, even as they recognize the emotional hole that can never be filled.
Florida does impose some limitations and procedural hurdles on damages (for instance, you have to itemize past vs. future damages, and certain types of damages might not be available for specific classes of plaintiffs in wrongful death cases Florida infamously bars adult children from recovering mental pain & suffering in medical malpractice wrongful deaths of parents, and vice versa, due to a controversial statute). However, if liability is proven, juries can and do award substantial sums to reflect the harm done. In the LabCorp Pap smear case, the jury’s total award was over $20 million, though reduced on post trial motions; in other cases around the country, multi million dollar settlements for lab errors (like missed cancer) are not uncommon.
Finally, beyond compensatory damages, Florida allows the possibility of punitive damages in malpractice cases if there is gross negligence or intentional misconduct. Punitive damages are not often pursued in straightforward misdiagnosis cases (they’re more common if, say, a lab was falsifying results or a doctor was drunk on duty egregious conduct). But if a pathology lab’s conduct was reckless for instance, knowingly using unqualified staff to save money at the expense of accuracy then punitive damages could be sought to punish and deter such behavior. Florida caps punitive damages generally at the greater of $500,000 or 3x the compensatory damages, with some exceptions.

Empowerment and Next Steps for Affected Patients
Suffering harm from a medical lab’s mistake can leave patients feeling shocked, betrayed, and unsure where to turn. The situation may feel very clinical a slide was misread, a report misfiled yet the impact on your life is deeply personal. It’s important to know that you do have rights and options. Florida’s system may be complex, but it is built to allow injured patients to hold healthcare providers accountable when they negligently cause harm.
If you find yourself in this unfortunate scenario, here are some empowering steps and considerations:
Trust Your Instincts and Seek Answers
Many malpractice cases begin with a patient saying “something just felt off.” If you were told for months that nothing was wrong while your health deteriorated, or if a new doctor looks at your old tests and immediately catches an error, don’t be afraid to ask questions. Hospitals and labs should have internal processes to review possible diagnostic errors.
You can request copies of your pathology slides or test results and seek a second opinion review. (In fact, in complex diagnoses, getting a second pathology review is common and can be life saving.) In Rex Morgan’s case, it was his persistence in having the 2011 slide re reviewed that unveiled the mistake. You are your own best advocate and early action on your part might mitigate damage or at least uncover the truth sooner.
Consult a Qualified Medical Malpractice Attorney
As should be evident by now, navigating a pathology malpractice claim in Florida requires legal and medical sophistication. An experienced Florida malpractice attorney can evaluate your case (often with an initial free consultation) and help obtain the necessary medical expert reviews. They will know the pre suit rules, deadlines, and how to properly frame the case. Malpractice law has numerous traps for the unwary you need someone who knows how to meet the notice requirements, how to secure top notch experts, and how to counter the defenses that labs will raise.
Moreover, malpractice cases are usually taken on a contingency fee, meaning the lawyers are only paid if they recover money for you, and they front the expenses (like those costly expert fees). Given the high costs, they will only take cases with strong merit so if an attorney agrees to take on your pathology error case, it’s a good sign that your claim is considered valid. Don’t delay in seeking legal advice; remember the statute of limitations is running, and even the pre suit investigation itself takes time.
Preserve Evidence
If you suspect a lab error, make sure all relevant evidence is preserved. This includes the pathology slides, tissue blocks, lab reports, doctor’s notes, and any communications you had with providers. In Florida, you have a right to obtain your medical records. Your attorney can also send preservation letters to ensure a lab doesn’t destroy or “lose” the slide in question (pathology labs generally keep slides for a number of years e.g., 10 years for surgical pathology slides under CLIA regulations but it’s wise to secure them).
Those slides may need to be re read by an independent expert. Also, write down what you recall e.g., “On X date, I was told my biopsy was negative, then on Y date I was diagnosed with advanced disease.” A timeline can help clarify the sequence of events. Your pain and suffering should also be documented: keep a journal of how the delay or misdiagnosis impacted you emotionally and physically. This can be useful later for explaining damages.
Focus on Healing (but Don’t Forgo Justice)
Your health is paramount. Pursuing a legal case can be time consuming and emotionally draining, so ensure you have a support system. Family, counselors, or support groups (for example, cancer survivor groups) can provide understanding and comfort. At the same time, holding a negligent lab accountable can itself be empowering. Many patients say that knowing their lawsuit might prompt improvements better protocols, double reading of slides, etc. gives meaning to an otherwise senseless tragedy.
It’s not about revenge; it’s about preventing others from suffering the same fate. Florida malpractice suits often lead hospitals and labs to implement new safety measures. For instance, after some high profile Pap smear misses, labs instituted policies where two cytotechnologists must review each slide, or an automated imaging scan assists in finding abnormal cells.
While your primary goal is rightful compensation for your losses, a side effect is potential systemic change. As one patient’s family said, “Enough is enough. It’s time to start saving lives” suing can send that message loudly.
Understand the Challenges
It’s also important to enter the process with eyes open. Labs and their insurers fight these cases hard. They often argue that pathology is as much art as science and that the error was a “reasonable miss” or an unavoidable accident. They may contend that the harm was inevitable due to the disease itself, not the timing of diagnosis.
You should be prepared for a battle of experts it might be disconcerting to hear a defense expert suggest that no pathologist could have done better, or that your cancer was incurable anyway. Trust in the evidence and your own expert.
Not every malpractice case in Florida wins; some are lost if juries believe the doctor’s side or find no negligence. However, by thoroughly preparing and understanding your case, you maximize your chances. Florida juries have shown they will absolutely hold labs liable when presented with clear evidence of negligence leading to harm.
Stay Empowered and Informed
The legal journey might be long (malpractice cases can take a couple of years or more, especially if they go to trial). But knowledge is power. Ask your attorney to explain each step. When you get to deposition or trial, you will have the truth on your side you know what you went through, and now you know how it happened and that it shouldn’t have happened.
Many patients find a degree of closure in simply uncovering exactly where the error occurred (was it a misread slide? A mixed sample? Who was responsible?). That clarity can replace nagging questions with concrete answers. And if negligence is established, holding the wrongdoers accountable can provide a sense of justice.
Conclusion
In summary, pathology lab malpractice is a serious issue that Florida law addresses through a combination of patient rights and procedural safeguards. If you’ve been harmed by a lab’s mistake, you are not helpless. You can demand answers; you can pursue compensation for your losses. The road has requirements expert support, pre suit notice, proof of each element but with diligent legal help, those hurdles are surmountable. Florida’s system, while strict, is ultimately designed to help those truly wronged to find relief. By learning about the process, you’ve taken an important step toward regaining control.
No one can rewind time and undo the pain caused by a diagnostic error. But by seeking legal recourse, you can secure resources to cope with the aftermath and perhaps spur changes that protect others. In the wake of a pathology error, it’s natural to feel overwhelmed yet, as this guide hopefully shows, there is a path forward. You have the right to answers, accountability, and compensation, and the Florida legal system provides a mechanism to attain them. Empower yourself with that knowledge, and don’t hesitate to reach out for professional help to assert your rights under the law.
Attorney Bio: Jorge L. Flores, Florida Bar No. 53244, has been representing families in Miami Dade for over 30 years.
Disclaimer: This overview is general information, not legal advice. Deadlines and procedures can change based on facts and parties. For guidance on your specific situation, contact a Florida medical malpractice attorney.
