Introduction: When Vigilance Fails
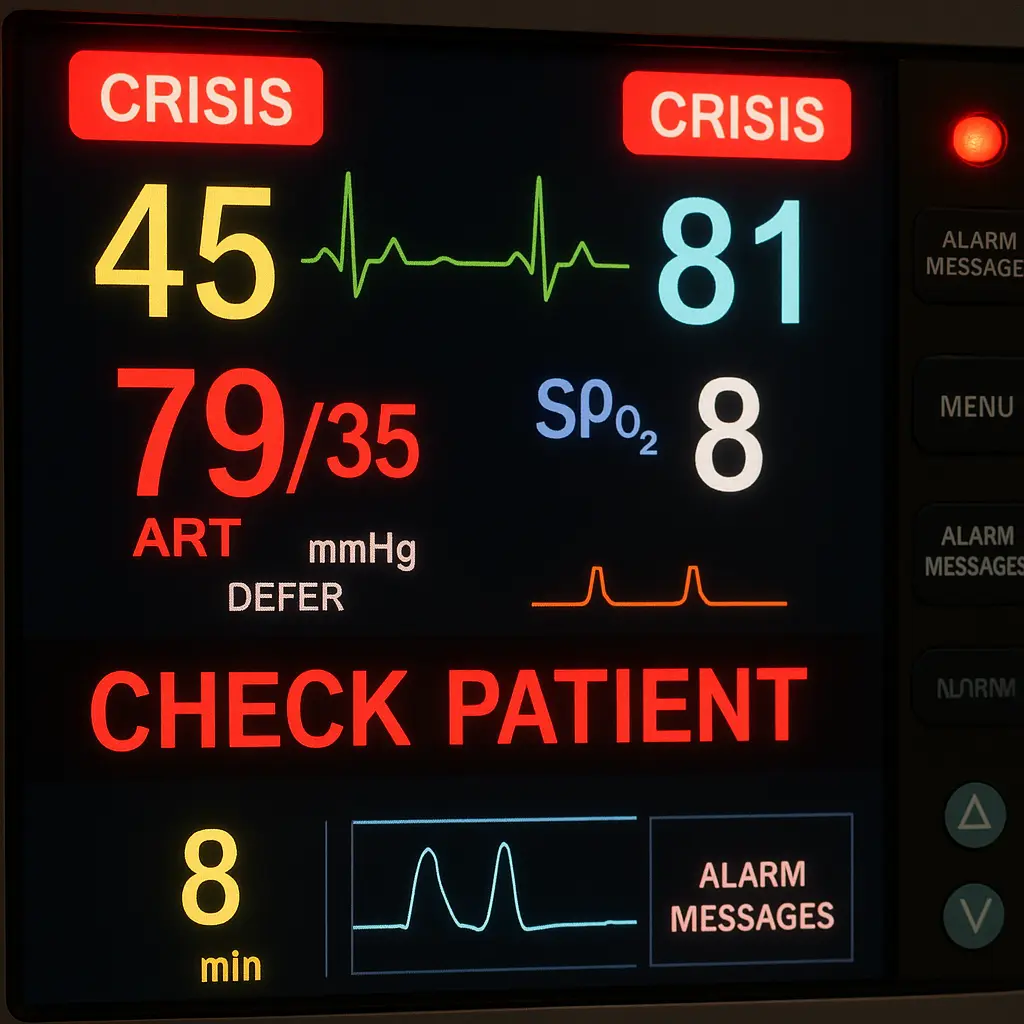
Imagine your loved one is recovering from surgery in a Florida hospital. The room is quiet except for the rhythmic beeping of monitors tracking their vital signs. Suddenly, one of the monitors flashes a critical alarm heart rate plummeting, oxygen levels dipping dangerously low. Minutes pass, but no nurse rushes in. The alarm continues its urgent screech unheeded. By the time help finally arrives, your loved one is unresponsive. This nightmare scenario is the result of a failure to monitor a preventable and often deadly form of medical error.
For families, the emotional toll of such an incident is immeasurable. You trusted the hospital to watch over your relative’s recovery, only to find that critical warning signs were ignored or missed. Failure to monitor malpractice refers to healthcare providers neglecting the essential duty of observing a patient’s condition, whether after surgery or during a general hospital stay. It can mean vital signs like blood pressure, heart rate, or oxygen saturation were not checked regularly. Alarms might have been silenced or overlooked, or symptoms and patient complaints brushed aside. In short, the medical team failed to catch a worsening problem in time, and the results can be devastating.
What Counts as a Failure to Monitor?
Failure to monitor is broader than a single missed vital sign it encompasses any scenario where doctors, nurses, or hospital staff don’t adequately keep track of a patient’s condition when they should. Common examples include:
Ignoring Monitor Alarms
Modern hospital bedsides are equipped with monitors that beep or flash when a patient’s vitals go outside safe ranges. If those alarms are ignored or turned off, critical events like a drop in oxygen or a spike in blood pressure can go unnoticed. Alarm fatigue when staff become desensitized to frequent alarms has been linked to hundreds of patient deaths nationally. There is simply no excuse for silencing an alarm without ensuring the patient is safe.
Not Checking Vitals and Signs
Patients in recovery or under heavy medication need periodic checks. For instance, after surgery, nurses should measure blood pressure, pulse, respiration, and temperature on schedule. If they fail to do these routine checks, they might miss signs of internal bleeding or infection until the patient collapses.
Delayed Response to Distress
If a patient is visibly in distress struggling to breathe, in extreme pain, or unusually drowsy a timely intervention can save their life. A failure to monitor includes situations where staff notice these signs too late or not at all. For example, a patient on opioid painkillers might show signs of respiratory depression (slow, shallow breathing) that require immediate action. Ignoring those signs can lead to a preventable respiratory arrest.
Improper Charting or Handoff
Hospitals rely on accurate charting and communication. If one shift doesn’t properly record a patient’s declining status or fails to tell the next shift, the patient may effectively go unmonitored for hours. Vital information falling through the cracks is another form of monitoring failure.
In all these examples, the standard of care what a reasonably careful medical provider would do is not met. Medical staff have a duty to continuously observe and react to a patient’s condition. When they breach that duty by not monitoring properly and the patient is harmed as a result, it constitutes medical malpractice.
Post Operative Monitoring vs General Inpatient Care
Patients are especially vulnerable right after surgery. Post operative monitoring failures occur when staff do not watch a patient closely during the hours and days following an operation. In this period, complications can strike suddenly:
Post Operative Complications
Internal Bleeding
A surgical patient might develop internal hemorrhage. If nurses aren’t monitoring blood pressure, heart rate, and abdominal signs, internal bleeding can progress until the patient goes into shock. By the time the issue is obvious, it may be too late to save them.
Blood Clots
After surgery, immobility or tissue damage can lead to blood clots (deep vein thrombosis). If warning signs like swelling, pain in a limb, or dropping oxygen levels (from a clot traveling to the lungs) are not spotted through proper monitoring, the clot could cause a deadly pulmonary embolism or stroke.
Reaction to Anesthesia/Pain Medication
Post operative patients often receive strong pain medications (opioids) or may still be affected by anesthesia. These drugs can depress breathing. That’s why close monitoring is non negotiable when opioids are administered. In one Florida case, nurses removed a patient’s monitors too soon after surgery. The patient had been given high doses of Dilaudid (a potent opioid) and showed signs of slowed breathing, but staff failed to intervene. The patient was later found unresponsive and suffered brain damage due to lack of oxygen.
General Inpatient Monitoring Failures
General inpatient monitoring failures refer to negligence in watching over any hospitalized patient, not just those recovering from surgery. This can happen in emergency rooms, on regular hospital floors, or in intensive care units:
Ignored Vital Changes
Even outside the post op context, patients with conditions like heart problems, infections, or breathing issues need vigilant monitoring. In an ICU, even slight changes in heart rhythm or oxygen saturation can signal a life threatening emergency. But those subtle warnings matter only if someone is paying attention.
Neglecting Alarms and Equipment
General care areas also use telemetry (heart monitors), pulse oximeters, and other devices. If a patient is placed on a heart monitor but the readings aren’t actively watched, a lethal arrhythmia could be missed. For example, failing to monitor a heart attack patient’s telemetry could mean nobody notices when they go into cardiac arrest.
Overlooking Symptoms of Infection or Sepsis
Hospital patients can develop infections like a surgical site infection or pneumonia. Nurses are supposed to monitor temperatures, lab results, and other indicators closely. If a fever, rising heart rate, or dropping blood pressure (all potential sepsis signs) is recorded but ignored, a localized infection can turn into full blown septic shock.
Inadequate Psychiatric Supervision
Even though this article focuses on medical/surgical contexts, it’s worth noting that in psychiatric units a failure to monitor can mean not watching a suicidal patient or not checking on someone under sedation. The results self harm, violence, or other injuries are just as devastating. Florida law recognizes that hospitals and staff have a high duty of care in these settings. If that duty is breached and harm occurs, it may amount to malpractice.
Both post operative and general monitoring lapses can lead to the same heartbreaking outcomes. The primary difference lies in when and where the negligence happens: right after a procedure versus during routine inpatient care. In either case, the key point is that a healthcare provider who should have caught a problem failed to do so.
Real Florida Case Examples: Tragedies from Lack of Monitoring
Real life cases illustrate how catastrophic a failure to monitor can be. Florida courts have seen numerous instances where patients were permanently injured or lost their lives due to simple inattention:
Post Surgery Opioid Overdose $7.9M Verdict
A Miami area hospital was ordered to pay $7.9 million after a post operative patient suffered irreversible brain damage. The patient had undergone surgery and was on high doses of painkillers (Dilaudid and morphine). Nurses removed his vital sign monitors and left him essentially unobserved. He showed signs of respiratory depression (extremely slow breathing) a known risk with those medications but no one responded in time. The man was found unresponsive and never woke up, passing away two years later. This case tragically shows how a few hours of neglect can cost a life. It highlights that hospitals must prioritize monitoring when a patient is recovering from surgery and on powerful medications.
Untreated Sleep Apnea & Painkiller Fatality $20M Jury Award
In another Florida case, a 53 year old man was hospitalized for pancreatitis and given an unusually high dose of the opioid Dilaudid for pain. The doctor failed to ask about the patient’s sleep apnea a condition that makes opioid use far riskier and crucially failed to put the patient on any oxygen or heart monitor. Nurses did not closely watch his breathing overnight.
By the next day, the man’s heart had stopped in his hospital bed. Although doctors resuscitated him, he had been without oxygen for too long and suffered profound brain damage, remaining in a coma until his family removed life support. A South Florida jury ultimately awarded $20 million to his wife and young son for this egregious negligence.
At trial, experts testified that not monitoring a patient on such a high opioid dose was a clear breach of the standard of care. The verdict sent a strong message that ignoring basic monitoring protocols can have dire consequences.
These cases are not outliers. For families who endure such outcomes, the overriding feelings are shock and anger “How could this happen in a modern hospital?” The unfortunate reality is that systemic issues like understaffing, poor training, and alarm fatigue often play a role. From the patient’s perspective, however, it still feels like a profound betrayal of trust.

Visually, a failure to monitor might look like a nurse dismissing a flashing alarm or a patient chart left unchecked at the foot of the bed. The human side of that image is a family in anguish at a bedside a loved one on a ventilator or a patient who never got the chance to recover. No family ever expects to lose someone dear because a caregiver failed to watch the monitors or respond when help was needed.
Injuries and Harm Caused by Monitoring Failures
When medical staff fail to monitor properly, the resulting harm can be severe and often permanent. Some of the serious injuries and medical emergencies tied to monitoring failures include:
Brain Damage from Lack of Oxygen
If a patient’s declining respiration or airway blockage isn’t noticed, the brain can be deprived of oxygen (hypoxia). This can occur in post op patients on narcotics or sedatives. Brain injury due to oxygen loss can leave a person in a vegetative state or with permanent cognitive impairment.
Cardiac Arrest
Unnoticed heart rhythm problems or untreated complications can lead to the heart stopping. Without immediate CPR and defibrillation, cardiac arrest is usually fatal or results in severe brain damage. Failing to monitor means missing the warning arrhythmias or blood pressure crashes that come before an arrest.
Sepsis from Untreated Infection
If nurses don’t monitor signs of infection (fever, high heart rate, low blood pressure, confusion), a patient’s localized infection can escalate to sepsis. Sepsis is a body wide infection response that can progress to septic shock, causing organ failure. Early detection through vital signs and labs is key negligence can let a treatable infection turn deadly.
Stroke or Blood Clot Complications
Blood clots can form in immobile patients (for example, after orthopedic surgery). If a clot travels to the lungs it causes a pulmonary embolism; to the brain, a stroke. Monitoring oxygen levels, limb swelling, and neurological status can prompt quick intervention (like administering blood thinners). Missing these signs means the first “warning” might be a catastrophic collapse.
Respiratory Failure
Especially in cases involving pain medication, anesthesia, or sedation, a patient can slip into respiratory failure (when breathing slows or stops). This may happen during recovery while the patient is on opioids or under sedation for a procedure. Continuous monitoring of oxygen saturation and respiratory rate is standard if it’s skipped, the patient can quietly stop breathing.
Wrongful Death
Ultimately, any of the above scenarios can lead to the patient’s death. When someone dies because no one was watching when they should have been, it may be considered a wrongful death caused by medical negligence.
Each of these outcomes is a nightmare for patients and their families, made worse by knowing that timely attention likely could have prevented it. Patients trust that in a hospital, professionals are “on guard” for such dangers 24/7. A failure to monitor betrays that trust, leaving the patient unprotected when they are most vulnerable.
Florida’s Medical Malpractice Process for Negligent Monitoring
Florida has specific laws to help patients and families seek justice for medical malpractice including cases of failure to monitor. However, the process is complex and different from ordinary injury lawsuits. Here are the key steps and rules to know:
Two Year Statute of Limitations
In Florida, you generally have 2 years from the date of the injury or from the date you discovered (or reasonably should have discovered) that malpractice occurred to file a lawsuit. There is also an absolute deadline of 4 years from the date of the malpractice (called the statute of repose), after which you cannot bring a claim. However, if a provider concealed the negligence (for example, through fraud), the window can extend up to 7 years. Additionally, for minors injured before age 8, the law may allow claims until the child’s eighth birthday in many cases. These time limits are strict. Missing the statute of limitations will likely bar your claim, so it’s crucial to act promptly and consult an attorney as soon as you suspect malpractice.
Pre Suit Investigation and Expert Affidavit
Florida requires malpractice victims to go through a pre suit process before filing a lawsuit. You must first obtain a sworn opinion from a qualified medical expert (usually a doctor in the same field) who has reviewed your records and believes negligence likely occurred. This expert review (often formalized as an affidavit) essentially confirms your case has merit. It must detail how the healthcare provider violated the standard of care for example, by failing to monitor appropriately and how that failure caused your injury. Your attorney will help find a suitable expert. Without this supporting expert opinion, you cannot proceed with a malpractice claim in Florida.
Notice of Intent and 90 Day Waiting Period
Once the expert has backed your claim, your lawyer serves a Notice of Intent to Initiate Litigation on each prospective defendant (the hospital, doctor, or staff member). This notice outlines your allegations and includes the expert’s affidavit. After the notice is delivered, Florida law imposes a 90 day presuit period during which no lawsuit can be filed. This gives the hospital or provider a chance to investigate and respond. The statute of limitations is tolled (paused) during these 90 days. The hospital or doctor must respond within that 90 day window. They will either (a) offer to settle, (b) propose arbitration, or (c) reject the claim. If they deny liability or if 90 days pass with no resolution, you are then free to file the lawsuit in court.
Filing the Lawsuit and Litigation
After the presuit period, if the claim isn’t resolved, your attorney can file a formal complaint in civil court. The case then proceeds through the typical litigation stages the defendants file responses, both sides exchange evidence (discovery), expert depositions are taken, and the case may go to trial if not settled. Keep in mind that Florida malpractice cases often involve a “battle of the experts.” Your side will present medical experts who testify that the failure to monitor was a clear breach of the standard of care that caused the injury, while the defense will have its own experts claim either no negligence or that the outcome was unavoidable. These cases can be complex. That is why having a lawyer experienced in Florida’s medical malpractice laws is critical.
Throughout this process, a knowledgeable Florida medical malpractice attorney will guide you and handle the procedural hurdles. Florida’s presuit requirements the expert affidavit and notice are designed to encourage early resolution and weed out frivolous suits, but they also add steps that can be daunting for victims. An experienced lawyer ensures all deadlines are met and paperwork is done correctly while you focus on healing and family.
How an Experienced Lawyer Can Help After a Monitoring Failure
Navigating a medical malpractice claim is challenging, especially when you’re dealing with the physical and emotional fallout of a medical tragedy. An experienced malpractice lawyer serves as both your advocate and your guide. Here are a few ways they can help:
Investigation
Your legal team will work quickly to gather medical records, monitor logs, and hospital policies to understand exactly what happened. In a failure to monitor case, they look for gaps in nursing notes, missed vital sign entries, malfunctioning equipment, or ignored alarm data. They may also investigate whether the hospital had prior safety issues (for example, a history of alarm failures or understaffing at critical times).
Expert Support
Attorneys connect with medical experts such as critical care nurses, anesthesiologists, or surgeons who can review the care you received and testify about what should have been done differently. These experts are essential for proving that the lack of monitoring was a deviation from the standard of care.
Building the Case
Your attorney will compile evidence to show the chain of causation how the lack of monitoring led directly to the harm. For instance, they might demonstrate that “if the nurse had checked the patient’s vitals at 2:00 AM, they would have seen a drop in blood pressure indicating internal bleeding, and timely surgery could have saved the patient.” This kind of explanation connects the dots clearly for a judge or jury.
Empathy and Communication
A skilled lawyer understands the emotional toll on families. They will handle all communication with the hospital and insurance companies so you don’t have to relive the trauma repeatedly. You’ll be kept informed at each step whether it’s the presuit investigation or preparing for a deposition without being overwhelmed by legalese.
Maximizing Compensation
While no amount of money can undo a life altering injury or loss, holding the negligent parties financially accountable is how civil law provides justice. A malpractice claim can seek compensation for medical bills, rehabilitation costs, lost income, and the very real pain and suffering you’ve experienced. In a wrongful death case, damages may include funeral expenses and the family’s loss of companionship and support. Your lawyer’s job is to pursue the full compensation you deserve under Florida law, and even to seek punitive damages if the conduct was egregious.
Emotionally, taking legal action is also about finding answers and closure. Hospitals rarely volunteer an admission of fault when a patient is hurt or dies under their watch. Families are often left with painful what ifs: “Would Mom still be alive if someone had checked on her?” or “Why didn’t they respond to that alarm?” A malpractice claim forces a thorough review of what went wrong. In some cases it leads to policy changes so that future patients are monitored more carefully. It also brings a sense of accountability knowing that those responsible face consequences which can help families in the healing process.
Holding Florida Healthcare Providers Accountable
Medical professionals and hospitals in Florida are held to high standards for patient care. Monitoring a patient’s condition is one of the most fundamental duties of any healthcare team. When this duty is neglected, the results are often tragic but the law provides a path for recourse. Florida’s legal system, through malpractice claims, enables injured patients or grieving families to demand answers and compensation when a provider’s inattention causes harm. The goal is not only to recover damages, but also to shine a light on negligence so that it doesn’t happen to someone else.
If you suspect that you or a family member suffered needless harm because medical staff failed to monitor properly, know that you are not alone and that you have rights. Start by consulting a qualified Florida medical malpractice attorney who can evaluate your case with compassion and expertise. They will explain how the law applies to your situation and what steps to take next.
Every patient deserves vigilant care. When hospitals and staff fall short ignoring vital signs, missing alarms, or delaying intervention until a crisis they must be held accountable. By understanding both the medical and the legal aspects of a failure to monitor malpractice case, you can make informed decisions to protect your family’s future. In doing so, you help pursue justice for the preventable harm you’ve endured.
Attorney Bio: Jorge L. Flores, Florida Bar No. 53244, has been representing families in Miami Dade for over 30 years.
Disclaimer: This overview is general information, not legal advice. Deadlines and procedures can change based on facts and parties. For guidance on your specific situation, contact a Florida medical malpractice attorney.
